Hey everybody, I’m back.
We’re going to switch gears and talk about gastroesophageal reflux disease (GERD). If you think IBS (irritable bowel syndrome) is common, GERD may be even more ubiquitous, affecting roughly 1 in 5 people. These are the questions people are asking. This is why you turn to Dr K for answers.
You might ask, what is GERD? Quite simply, it is the movement of stomach fluid or contents, which tend to be acidic, into the esophagus. This often results in symptoms such as heartburn or chest pain, but can also occur silently (shhhhh!) and cause damage to the mucosa (the lining of the GI tract). OK then, what do you mean by heartburn? Well, as I always used to say, if you’ve got it, you know it. Usually a burning sensation in the middle of your chest after eating (think spicy!) or maybe a pressure sensation or a just doesn’t feel right kind of a feeling.
How do doctors diagnose GERD? It’s not as easy as you might think. Burning doesn’t always mean GERD. There are characteristic findings on endoscopy (erosions or ulcers) but not everyone has them. Your doc might try you on a PPI medicine (like Prilosec) for 8 weeks before doing a scope. These meds reduce stomach acid; if your symptoms go away, that’s pretty good evidence that acid coming up into your esophagus is the problem. There is also this test with a tube in your nose for 24 hours, but…
Maybe we should take a sec to review the anatomy. The esophagus and stomach come together at the GEJ (gastroesophageal junction). Kinda like the US-Mexico border. Or Russia and the Ukraine.
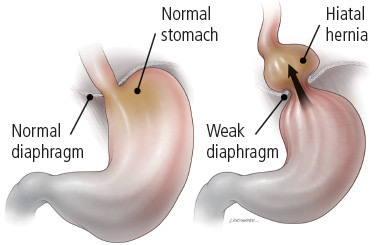
The GEJ is supposed to stay closed most of the time, keeping the stomach juice in the stomach and out of the esophagus. When you swallow, the GEJ opens to let the food through and then closes again (the one-way valve analogy you may have heard). Sometimes, the GEJ is just loose. Or the LES (lower esophageal sphincter; that’s the actual muscle at the junction, the “valve”, if you will)) opens up now and again when it’s supposed to be tight. Or you might have a hiatal hernia- that’s another concept that’s often misunderstood.
With a hiatal hernia (HH), the top of the stomach is above the diaphragm and thus in the chest. Most hiatal hernias are small, as depicted above on the right, about one inch in length. When the LES is in the chest, it tends to have less tone, allowing reflux to occur. Small HHs usually do not need to be fixed and we treat the reflux with medication and lifestyle changes. Large hiatal hernias, where a third or more of the stomach is above the diaphragm, are another animal. These are much less common. Depending on the symptoms (heartburn vs regurgitation) meds alone can work, but sometimes, surgery is needed.
So how do we treat the symptoms of GERD? Start with common sense, like watch what you eat, keep your weight down, don’t smoke. Medications like PPIs (proton pump inhibitors like omeprazole, Nexium, pantoprazole) and H2 blockers (like Pepcid or famotidine) work by reducing the amount of acid your stomach makes after you eat. Remember, it’s the acid that causes most, but not all, the symptoms and tissue damage
Are PPIs safe? Don’t we need stomach acid for health and digestion? The short answers are yes and no. The whole PPI story is a huge topic for another day. We always look at medical decisions through a risk/benefit lens. The theoretical risks of PPI are really very low (really) and the benefits huge. So take your PPI if you need it or have a condition that requires it like erosive esophagitis or Barrett’s esophagus. I take my PPI every day. Periodically, I try to come off it but after a day or two, my heartburn comes back, so I go back on it. Because I don’t like heartburn. We call that quality of life.
Hold on, what was that Barrett’s esophagus thing? Good question, I’m glad to see you’re paying attention! A minority of people with GERD will develop what we call complications. These include erosive esophagitis, strictures (narrowing of the esophagus from scar tissue that may occur with healing), Barrett’s and cancer (specifically, adenocarcinoma) of the esophagus. These potential complications are a big reason why your GI doc will recommend an endoscopy (upper scope) at some time, especially if you have had GERD symptoms for several years. If your esophageal mucosa looks pretty normal (no erosions or ulcers), you probably will never get any of the aforementioned complications. Yea! You’re a NERD! Or more accurately, you have NERD (nonerosive reflux disease). Whatever it takes to ease your symptoms- lifestyle changes, antacids (I love Gaviscon, btw), H2B or PPI- that’s what you do. It’s truly up to you, you and your esophagus.
But if you have Grade C or D erosive esophagitis, only PPIs will heal your poor mucosa. And if it doesn’t heal, that increases your chances of developing strictures or cancer. So, in this situation, you really should take your PPI every day, even if your symptoms are not that bad. Benefit WAY outweighs risk.
Barrett’s esophagus is a change in the lining of the esophagus that can develop after years of acid reflux. I mentioned earlier that the esophagus tries to heal itself after being repeatedly injured by acid. Besides scarring, the tissue type lining the esophagus may actually change. This is called metaplasia; the same concept occurs in other parts of the body, such as the cervix. The problem with metaplasia is it can transform into carcinoma. Some people may be genetically predisposed, but the biggest at risk group for cancer in Barrett’s patients appears to be overweight, white men. If you are a woman with Barrett’s, your risk of developing esophageal cancer with Barrett’s is pretty low. Not everyone with Barrett’s needs to be scoped regularly to look for dysplasia. Be sure to have an honest discussion with your gastroenterologist about your risk and what’s best for you.
That’s a quick spin through a big topic. I tried to hit what I think are the highlights. Get a good doctor and follow her or his advice. You’re not alone, there are lots of us refluxers out there. Even if you are a NERD 🙂