Hello again. Today’s topic is a term I’m sure you have heard at one time or another, diverticulitis. But what the heck is it? “Some kind of bowel thing, right?” Well, sure, but can you be more specific? “It’s when the pockets in your intestine get inflamed.” Ahh, now we’re getting somewhere! Did you ever have an uncle who would say, as you passed him the creamed corn at Thanksgiving, “no thanks, kid, my diverticulitis is acting up again”? You did? I’m not surprised; diverticulitis (or d-itis, for short) is among the ten most common digestive conditions. Common, but also one of the more misunderstood disorders we deal with in GI. Not as “sexy” as say, Crohn’s disease, but at times, equally perplexing, refractory and recalcitrant. Today I will try to explain what diverticulitis is, how we treat it, and things you can do to mitigate your risk.
Let’s start with semantics. “So, Doctor, do I have diverticulitis? Or is it diverticulosis, that’s what my CT report says.” Diverticulosis refers to those little “pockets” (one of my least favorite descriptors in all of medicine, btw) that occur in the wall of the bowel. Take a good look at Figure 1, see the little bulges (is bulge really better than pocket?). One bulge is called a diverticulum; more than one, diverticula.

Endoscopic appearance of sigmoid diverticulosis
We don’t know exactly why diverticula occur, but they are way more common in people eating diets low in fiber and high in fat content. In other words, the typical American diet! 60% of people above 60 years old in the US have this condition, most of them don’t know it unless they were told so after a screening colonoscopy.
The suffix -itis in medicine signifies inflammation of that tissue; -osis means simply the presence of a condition. Just as pancreatitis connotes inflammation of the pancreas, diverticulitis is inflammation of a segment of bowel (usually colon) containing diverticula. In western countries, diverticular disease is most often seen in the left colon (sigmoid and descendinig); occasionally the entire colon has “tics”.
Out of the millions, literally, of people with diverticulosis, only 2-5% will develop the painful condition of d-itis. “That occurs when a seed gets stuck in a pocket, right?” Well, no. We don’t really know what causes the inflammation to begin. This old theory posits that a particle of corn or nut gets stuck in a “pocket”, trapping stool there and then bacteria works its way past the lining and into the wall of the bowel, leading to inflammation/infection. Well, it’s not that straightforward, like a lot of things in medicine. In fact, there is strong evidence disproving this notion.
A fascinating study (1) was published in 2008, in which 47,000 men were followed for 18 years. The ones that ate the most popcorn/nuts/corn were the least likely to develop diverticulitis! (after controlling for all other variables). For real! Another old wives’ tale down the proverbial shitter! And yet, as many as 50% of physicians and surgeons still, to this day, tell their d-itis patients to avoid nuts and seeds forever. This advice deprives people of foods important in the Mediterranean diet, high in protein, fiber and antioxidants. So eat your cashews and almonds if you like them. Creamed corn, too. Just remember, as we’ve said before, moderation, moderation, moderation. And if you are convinced nuts and seeds give you pain or will cause a “flare”, that is your choice.
What we do know is, once you have your first episode of acute diverticulitis, you have an 8% likelihood of a recurrence in the first year. If you can get past that first year, the odds start to diminish. Recurrences are more common if you: are overweight, smoke, don’t exercise regularly (we’re talking about 2 hrs/week, not exactly training for a marathon), eat a low fiber/high red meat diet, and very importantly, take NSAIDs (like ibuprofen) regularly. So, kinda like the advice for fatty liver, there are some lifestyle choices you can make to prevent a recurrence. More salads, keep moving, maybe lay off the Advil. Probiotics do not prophylax against recurrent diverticulitis, there is no magic bullet. Just keep doing the hard work, if you are able.
What are the symptoms of diverticulitis? As Clubber Lang put it so eloquently in Rocky III, “P-A-I-N”. Typically in the left lower abdomen. It can be mild to severe, but it is fairly constant for at least several days. There often is some change in bowel habits, harder to pass stool and the stools tend to be smaller and thinner. The stools should not be bloody in acute diverticulitis. (Just so you know, there is something called diverticular bleeding, a painless and common cause of lower GI bleeding, not related to inflammation. A whole different animal.)
The diagnosis is suspected on symptoms and physical exam, and confirmed with characteristic findings on a CT scan of the abdomen. We call it severe if there is a LOT of inflammation and swelling, the WBC (white blood cell count) is very high (>15-20K), or if the patient is just plain old sick (I know, technical medical term, AKA clinical judgement). We call d-itis complicated if there is evidence for a perforation or obstruction. A small tear or leak (these can be quite tiny) can develop in the weakened bowel wall, allowing bacteria to get outside the friendly confines (CUBS reference) of the gut, resulting in an abscess (collection of pus, more on this later).
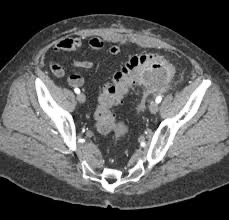
Acute diverticulitis with focal abscess on CT
Mild, uncomplicated diverticulitis can be treated as an outpatient. Traditionally, we have, and still do, prescribe antibiotics for all cases, but the times may be a-changin’. We have learned in the past decade that antibiotics do not hasten recovery or reduce complications in mild, uncomplicated cases. What, no antibiotics for diverticulitis? This is a big leap of faith for us, ahem, seasoned practitioners. But this applies only to young-ish, healthy people, a pretty small percentage of cases. Most people with d-itis are older and have other medical problems such as diabetes and cardiopulmonary disease; the immune response is not what it used to be, and antibiotics are needed to heal. If your episode is moderate to severe, you will spend some time in hospital on IV antibiotics. A small abscess can often resolve with antibiotics and time; larger ones usually need to be drained (by needle or operation).
“If I am diagnosed with acute diverticulitis, do I need a colonoscopy?” NOT early on, when you are having symptoms, definitely not. Colonoscopy in general is very safe, but the inflamed bowel is fragile, increasing the chances of a tear (perforation). There can be some exceptions to this, but the general rule is to wait until things settle down, 2 or 3 months. “Why do I need a scope, you all know what I have?” Good question. Once in a great while, a colon cancer can cause pain like this and look very similar on CT. Current guidelines state that if you have not had a c-scope in the 12 months preceeding your 1st bout with diverticulitis, get one after you are well.
So, when do we need to get the surgeon involved? The old adage was, after 2 or 3 episodes it’s time to remove that section of colon. But now it’s more like 4 or 5. Also important, however, is how severe the attacks are, how frequent, and also what does the patient want? Recurrent d-itis is a form of Russian Roulette (can we still use that metaphor?)- it can happen anytime and anywhere, home or abroad. Many folks, understandably, do not want to live under that threat. Surgeons prefer to operate on diverticular disease after the acute inflammation “cools down”, but may have to intervene ASAP with a perforation or a large abscess that the radiologist cannot take care of.
There’s a lot more stuff we can talk about re: diverticulitis, but I think that covers the gist of it. It can be straightforward and respond to treatment as expected, but it can also be sneaky and stubborn. The medical literature has described diverticulitis for the past 200 years, and yet it remains a challenge today. Nonetheless, there have been some remarkable changes in our approach in the past ten years or so, I think that’s very cool.
Happy Holidays, Everybody!
I dedicate this blog entry to a dear relative of mine who recently passed. She lived a very full life and was (still is) an inspiration to all who knew her and loved her. Rest in Peace, AJ.